Author: Meriel Tolhurst-Cleaver / Editor: Liz Herrieven / Reviewer: Katy Vose / Codes: R2 / Published: 08/05/2017 / Reviewed: 25/03/2025
It’s a common card to pick up in some paeds EDs – the yellow newborn. But whilst this can be an ‘easy’ one, such tiny babies can strike fear into the hearts of some! So a quick review of what to look for, and what not to miss, should keep us all calm when presented with a baby who looks like they could be auditioning for the Simpsons. Caveat: not all babies with jaundice look yellow. Of note babies with darker skin tones will not look yellow and it can be much harder to recognise that these babies are jaundiced. Look at their sclera or palms. You can also press lightly on the skin of their forehead/nose to detect yellow skin underneath.1
Listen to parents: they will have been staring at their newborn since birth and will know if they look different! They may however have brought the baby due to poor feeding/lethargy, etc. The second caveat is beware polycythaemic babies: these babies look plethoric, they are often the most jaundiced and therefore it is important not to miss them. They may also have tachypnoea, hypoglycaemia and lethargy.
When thinking about neonatal jaundice we can break it down into early (generally regarded as up to 14 days) and prolonged (over 2 weeks in term babies, or over 21 days in preterm infants). This post will look specifically at early jaundice.
Jaundice in the first 24 hours of life
Jaundice in the first 24 hours of life is ALWAYS PATHOLOGICAL and should be treated very seriously.
When you see it, think of sepsis, ABO/rhesus incompatibility or haemorrhage (e.g. subgaleal bleed). These babies should be seen and investigated quickly with a septic screen, FBC, Direct Coombs test and split bilirubin level, and referred promptly to the General Paediatric take for admission and management.
Early Jaundice after the first 24 hours of life
So, how do these babies present? They are usually between day 2 and day 6. and may present with a history of increasing, or newly noted jaundice.
Aside from jaundice, these babies may also have features such as lethargy (not waking for feeds), poor feeding (not interested in, or falling asleep whilst feeding), reduced wet and dirty nappies, or excessive weight loss.
So, how should you approach these patients? Start by congratulating the parents on the birth of their baby and be aware that they are probably exhausted and anxious.
History
- birth history
- previous children/history of jaundice
- gestation
- birth weight
- risk factors for sepsis see NICE guideline2
- date and time of birth (youll need it to plot the bilirubin later)
- history of bruising (e.g. forceps delivery)
- method and amounts of feeding (in the first few days babies should be feeding every 3-4 hours including overnight, breastfeeds should last 20-45 minutes, for bottle fed infants you can calculate intake over 24 hrs, a rough guide is: Day 1 60ml/kg, D2 80, D3 100, D4 120, D5 onwards 150)3
- urine output and colour (newborn urine should be very light in colour and they should have approximately the same number of wet nappies as their age in days -see image below)
- stool frequency and colour (see image below)

Examination
- examine the baby from top to toe, preferably in natural light
- examination of the sclerae, gums and blanched skin is useful across all skin tones
- note whether the conjunctiva are icteric and how far down the body the jaundice is evident (it starts on the face and progresses downwards)
- features of sepsis such as irritability, floppiness, poor perfusion, tachycardia, tachypnoea or a raised/tense fontanelle
- listen to the heart and check the femorals (just in case you are the first to also pick up congenital heart disease)
- weigh the baby (totally naked) and calculate weight loss from the birth weight. Every hospital has a different guideline, but generally speaking if it is about 8-10% youll need to discuss the baby with the paediatric team. Even if their jaundice does not need treatment, these babies are often admitted for observation of feeds.
Investigations
If there are no red flags for sepsis in the history, and the baby examines well but has significant jaundice (i.e. you can see they are jaundiced) then NICE4 recommends you send the following (can be done via a heel prick test)
- a split bilirubin
- FBC-look at haematocrit
- Group and Direct Antiglobulin Test (DAT, aka Direct Coombs Test or DCT). All of these can be done with a heel prick.
- consider adding a G6PD if the baby is of appropriate ethnic origin.
- If there is significant weight loss 12% send a U&E (as hypernatraemic dehydration is common) and refer to paediatrics
- In any baby with poor feeding consider a blood sugar.
If there are any concerns for sepsis you need to have a low threshold for doing a full septic screen (blood, urine and CSF cultures) and commencing appropriate IV antibiotics. If in doubt, you can get advice from the paediatric team. Remember that newborns can have very vague features of sepsis and may not mount a fever or much of an inflammatory response on their bloods. Be concerned if anything is amiss with their observations, general handling or appearance. If their bilirubin level is okay but the baby is sleepy, not waking for feeds, not taking good amounts of milk, or has weight loss of more than 8-10%, they need to be referred to the paediatric team.
NICE has updated their guideline and it recommends the use of a bilirubinometer in the first instance rather than blood tests, if one is available. This is not accurate for babies <24 hours or less than 35 weeks gestation. This is great for use on the postnatal wards where they are doing hundreds of jaundice checks, but most EDs wont have one of these. So, a heel prick it is. If you do have access to a bilirubinometer device then check out the NICE guidance4 for when to use it and when it is contraindicated. This video5 shows how to use one.
Get the bloods done early and be warned that they clot very easily, largely because newborn babies have such a high haematocrit, but potential poor feeding and poor perfusion also doesnt help. If possible, get someone experienced to do the heel prick.
Once the bloods are back you need to download a gestation-specific bilirubin chart4 and plot the bilirubin at the appropriate time from birth (this is when you need an accurate time and date of birth from the parents). Get a second person to double check your plotting independently mistakes are common.
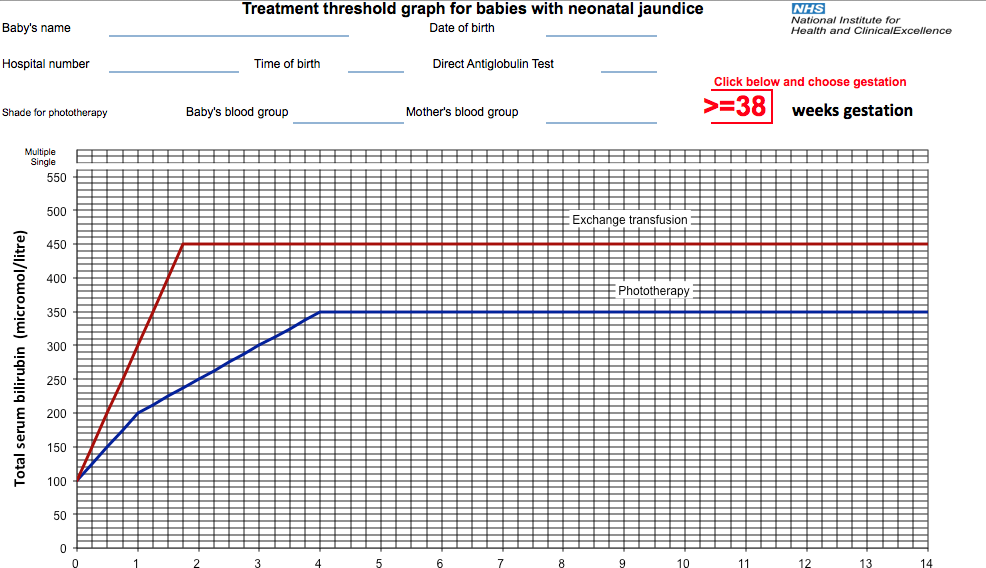
Remember that each little box on the chart is equivalent to 6 hours. If the bilirubin is above the treatment line, the baby needs admission for phototherapy, so refer to the General Paediatric take. If they are over the exchange transfusion line, they are at risk of kernicterus, seizures and coma. They need urgent phototherapy with as many light units as possible and IV fluids whilst an exchange transfusion is organised (this takes time), but get help early in view of this.
If the bilirubin is below the line then the family get to go home hurray! But bear in mind that if it is less than 50 micromol/l below the line youll need to organise for a further blood test within 18-24 hours (18 hours if there are recognised risk factors, which include sibling requiring phototherapy and exclusive breastfeeding). The NICE guidance4 has more information on this but also ask around locally as to whether the baby will have to return to ED or whether a community midwife could send a sample in. Other factors to consider when sending a baby home include whether you think the problem that has been causing the jaundice has been rectified, and whether the parents have a feeding plan/support for feeding in place there are usually local breastfeeding support groups that you can signpost them to. Do they have appropriate follow up with their midwife in the community to review the feeding/jaundice/weight gain over the next few days?
A quick reminder about performing split (sometimes called neonatal) bilirubin samples. The result will show the conjugated fraction, the unconjugated fraction and the total bilirubin level. A conjugated hyperbilirubinemia, where the conjugated fraction is 20% of the total level is often detected on a prolonged jaundiced screen (performed after 14 days). It is ALWAYS pathological, and usually represents hepatobiliary disease, such as biliary atresia. So, you should always check that the conjugated fraction is <20% of the total and if not the baby would need discussion with the paediatric team.
Causes of Jaundice
What causes the jaundice in these babies? Well, the first day list above is still relevant in the babies over 24 hours of age (so sepsis, ABO/rhesus incompatibility and haemorrhage should still be in the back of your mind). I personally use a conscious forcing strategy to mentally exclude sepsis whenever I see a jaundiced baby. There is more information about strategies such as this, and other ways to avoid bias, in this excellent podcast from Emergency Medicine Cases.6
Other causes include haemolysis, which should be picked up by your DAT or blood film; bruising or bleeding, which should be evident on examination; and G6PD deficiency test for this if you have any concerns. Most babies, however, will have physiologic jaundice or breast-milk jaundice. Whilst these are both diagnoses of exclusion, given the high incidence of jaundice in the newborn, NICE doesnt recommend doing more investigations than those listed above at first presentation. If the jaundice is prolonged, that is when you start to pull out the stops but you can read all about the investigation and management of prolonged jaundice in a separate blog on this site.
(Peer reviewed by Naomi Simmons)
References
- NHS UK – Newborn jaundice, diagnosis.
- National Institute for Health and Care Excellence (NICE) – Neonatal Infection. Quality Standard | Last updated: 23 January 2024.
- La Leche League International – breastfeeding information – frequency of breastfeeding.
- National Institute for Health and Care Excellence (NICE) – Jaundice in Newborn Babies Under 28 days. Clinical guideline | CG98 | Last updated: 31 October 2023.
- Bilirubinometer demonstration. linyanam video, YouTube 2011.
- Emergency Medicine Cases: Episode 75 Decision Making in EM Cognitive Debiasing, Situational Awareness & Preferred Error. 2016.
- Porter ML, Dennis BL. Hyperbilirubinemia in the term newborn. Am Fam Physician. 2002 Feb 15;65(4):599-606.

