Author: Govind Oliver / Editor: Charlie Reynard / Codes: / Published: 09/01/2020
Each year at the Royal College of Emergency Medicine (RCEM) Annual Scientific Conference, the prestigious Elizabeth Molyneux Prize is awarded. The prize, named in honour of Professor Elizabeth Molyneux, recognises outstanding work in the field of Paediatric Emergency Medicine (PEM).
It is not possible to do justice to Professor Molyneux in a few short lines. Her work, conducted over a lifetime dedicated to improving the care of children, includes: clinical care, teaching, research and collaboration in a spectrum of far-reaching and impactful global initiatives. Her research record contains an eye watering number of pier review publications including trials published in the Lancet. In short, she has both inspired and saved countless lives.
PEM is a fast growing sub-speciality within Emergency Medicine. Exciting research is being done by the PEM community with many following in the footsteps of Professor Molyneux. Here, we’ve put together a summary of the research, that was short-listed for the 2019 prize, with the hope of inspiring and encouraging those considering conducting research in PEM.
“Variability in Point Of Care Ultrasound (POCUS) practices in paediatric emergency departments in the UK & Ireland; a PERUKI study”
By Mark Lyttle et al., presented by Dan Magnus (Consultant in Emergency Medicine & Paediatric Emergency Medicine, University Hospitals Bristol)
POCUS is now embedded in adult emergency medicine. What about in PEM? The current practice of POCUS in PEM is unclear; as yet there is no standardised PEM POCUS curriculum, best practice standards or formal training courses. Mark and his colleagues set out to understand the variation in practice across the U.K.
Dan conducted a survey of the 63 sites in the Paediatric Emergency Research in the United Kingdom and Ireland (PERUKI) research network. A response for each was sought detailing the departments practices, hardware and major enablers and obstacles.
They obtained responses from 94% of those surveyed, which consisted of a mix of site and department types (e.g. 40% tertiary hospitals, 60% mixed adult/paediatric emergency departments and 30% Major Trauma Centres). The picture painted by these 59 sites is very clear:
- 90% of all sites had an ultrasound machine
- 70% reported some limited use by a small proportion of staff
- 100% had NO named POCUS lead
- 95% had NO teaching program or identified trainer
- Governance and practice is not currently standardised with routine documentation of findings in approximately half (55%) of cases, storage of images in 65% of images and over two thirds (68%) having no quality assurance measures.
The greatest enablers of PEM POCUS were its need, the access to funding for equipment, and clinician engagement. The greatest obstacles were the availability of training courses, trainers and the time to develop and maintain skills with the demands of current practice.
Dan and the team’s take home message:
Whilst hardware is available in most EDs, PEM POCUS is not yet widespread, with training being the greatest obstacle. Future work is needed to ascertain whether and how POCUS will be embraced in PEM.
Contact Dan about this work:
Contact Dan.Magnus@uhbristol.nhs.uk if you are interested in this research and would like to know more.
“Improving the documentation and communication for suspected non-accidental injury in children presenting to the Emergency Department following injury: a quality improvement study” Bby Chris Lowry (ST7 Paediatric Emergency Medicine, Royal Belfast Hospital for Sick Children)
Sadly non-accidental injury (NAI) continues to be a common cause for injuries in children, especially in the very young, immobile child. Recent data from the Scottish Trauma Audit Group (STAG) found that 8% of paediatric trauma cases, all children under the age of 2, were as a result of NAI. Any clinician reviewing injured children must consider NAI. In the words of J.K. Rowling’s character Mad Eye-Moody: “Constant Vigilance!”
Chris found through audit work at his local hospital that both the understanding and documentation of NAI was poor amongst clinicians. I would guess that Chris’s experience is not unique. Chris undertook a quality improvement study, which focussed on the implementation of three key changes within local practice:
- Creation of a tick-sheet pro-forma for documentation of key data for NAI for use in children presenting with injury,
- Formation of a new referral process to facilitate the sharing of information with social work,
- Set up of a new multidisciplinary child protection meeting to include staff from social work, paediatrics, child protection and emergency medicine.
These changes made some quite marked improvement in practice:
- Rise in clear documentation of child protection concerns from 0 to 70%
- Rise in documentation of who accompanied a child from 20 to 100%
- Rise in checking of social work involvement from 0 to 70%
- Increase in documentation of the time of an injury from 40% to 85%
Attendance at the child protection meeting dramatically improved and the number of sites has been expanded due to interest. Social work received 46 notifications of concern forms via the new referral process over the 9 months study period (3 for under 1s) all of which were deemed appropriate.
Chris’ take home message:
Having a standardised tick-sheet for NAI has markedly improved the consideration of NAI in children presenting with injury. Multi-disciplinary child-protection meetings have improved communication and collaboration between departments and improved the delivery of care.
Contact Chris about this work:
Contact Christopher.lowry@belfasttrust.hscni.net if you are interested in this research and would like to know more.
“Fluid Resuscitation of infant with sepsis”
By Lizzie Ryan (Paediatric Advanced Nurse Practitioner, Emergency Department, Kings College Hospital NHS Foundation Trust)
Clinicians working in paediatric emergency departments will be very familiar with the dangers of sepsis. It unfortunately remains a leading cause of mortality among children worldwide and stories of tragic cases often draw media attention.1 One of the key treatments we give to resuscitate infants with suspected sepsis is fluid. APLS positive clinicians will be familiar with the guidelines recommend 20ml/kg volume within the first ten minutes. However, following evidence from the Fluid Expansion as Supportive Therapy (FEAST) trial, a more restrictive approach may increasingly be being taken.2 The FEAST study was of course conducted in a low-income setting and questions around the applicability of its findings to our practice have been raised. The FiSH study highlights the challenges of conducting a similar study in high-income settings.3 Liz and her colleagues set out to review their local practice with a view to whether there was any correlation between the how much fluid was given in cases of suspected infant sepsis in their hospital.
Lizzi undertook a retrospective cohort study of infants with suspected sepsis presenting to the ED at an urban tertiary hospital. Data was collected regarding the volume, type, aliquots and timing of fluid, together with lactate levels. The acuity and length of admission were the measurable outcomes. In the 50 cases presenting between Nov.2015 – Mar.2018 only 50% of infants received fluid resuscitation at levels recommended in current guidance. Of these under resuscitated infants, 60% did not require any further fluid resuscitation. The admission length was under one week in the majority of cases (84%); there was no correlation between the initial fluid resuscitation practice and admission length. Only 2% of infants had positive blood cultures in this cohort.
Lizzi’s take home message:
In this small retrospective study, there were inconsistencies in fluid resuscitation practice. There was no apparent relationship between the initial fluid bolus volume and the length of stay. Further work is needed to explore clinician’s rationale for their choice of fluid bolus volume and whether a more restrictive approach should be advocated.
Contact Lizzi about this work:
Contact e.ryan1@nhs.net if you are interested in this research and would like to know more.
Can we make the Emergency Department handover safer?
By Yok Tan et al. (ST7 PEM Trainee, Birmingham Children’s Hospital)
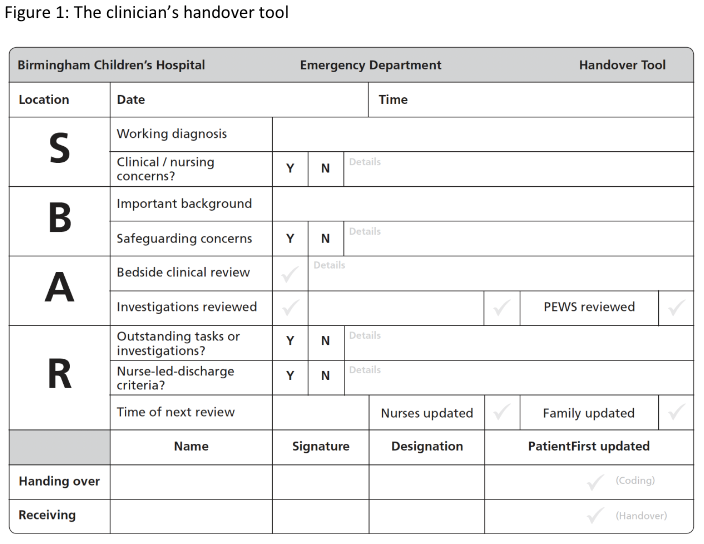
Handover of care is one of the most perilous procedures in medicine4. Never has this been more apparent than in the current state of overcrowded emergency departments and long bed waits. The nature of varying staff shift patterns, the high patient turnover and the ever changing patient volume and acuity compound the problem. The Situation, Background, Assessment and Request/ recommendation or SBAR method is a widely used communication tool.
Yok and his colleagues conducted a survey to examine the effect of implementing a standardised patient bedside handover tool for both clinicians and nurses. It was investigated for acceptance and adherence. The standardised tool would facilitate the safe continuity of care between shift changes and improve communication with patients and families.
The tool was designed, introduced and evaluated through a stepwise process for clinician and subsequently for nurses. It was created around the SBAR structure (the clinician handover tool is shown below). Of the 30 clinicians of varying grades surveyed, 90% felt use of the tool was safer for patients and 80% felt it should be rolled out within standardised practice. Qualitative data on clinician experience using the tool was captured. The main theme from clinicians was that they felt the tool made them do a more detailed and thorough handover. The nurses handover over tool received very positive feedback with comments that they were “happier” with handover and more satisfied to leave shift “without forgetting significant patient information”. As a result of the acceptability and perceived impact of the tool, both have become routine practice within their ED.
The Clinician’s handover tool
Yok’s take home message:
A simple formalised bedside handover tool incorporated into local standardised practice is accepted and used by both clinicians and nurses.
Contact Yok about this work:
Contact yok.tan@nhs.net if you are interested in this research and would like to know more.
Rectal Bleeding Presenting to the Paediatric Emergency Department
By Jordan Evans et al. (Paediatric Emergency Department, University Hospital of Wales, Cardiff).
Rectal bleeding is bread and butter in the adult population; I’d wager there is far less confidence amongst Emergency Physicians dealing with this presentation in the paediatric population. The differential diagnosis is wide, from the benign to life threatening and it will often accompany a tremendous amount of concern from the child’s caregivers. The current literature in the area is limited. Jordan and his colleagues aimed to: describe the frequency of this presentation, understand what the most common diagnoses were in these patients and describe what their management was.
They performed a retrospective case note review of all children presenting to a single urban paediatric emergency department (PED) at a tertiary hospital. They collected data on the child’s demographics, the diagnosis and care in PED and the diagnosis and care on follow-up. Over the two-year study period, 80 cases met their inclusion criteria. This amounted to 0.14% of all presentations to the PED. The average age of children presenting with bleeding per rectum was 5 years (3 months -15 years) with 51% female and 49% male.
- Collectively constipation and gastroenteritis accounted for 76% of diagnoses;
- 24% of children with PR bleeding were admitted the same day
- 38% were referred for outpatient follow up.
- Urgent intervention was required in only 5% of cases.
- There was agreement between PED diagnosis and outpatient diagnosis in 87% of cases.
Jordan’s take home message:
Bleeding per rectum is an infrequent presentation to the PED. The most common diagnoses are benign and many cases may be managed without need of admission or outpatient follow up. A high index of suspicion remains necessary to identify infrequent but serious pathology. There is currently limited evidence to guide practice and therefore further work is required.
Contact Jordan about this work:
Contact evans6651@doctors.org.uk, or on twitter @jordan_evans98, if you are interested in this research and would like to know more.
The inter-observer reliability of head injury assessment between clinicians and parents of head injured children
By Charlotte Kennedy et al. (Senior Clinical Fellow in Emergency Medicine and Academic Teaching Fellow, University of Lancaster)
It is easy sometimes to loose count of the number of children with head injury that are brought into the paediatric emergency department (PED). On occasion parents present because they have been told by nursery, school or another source of advice that they have to. Yet, 4 out of 5 children that we see have mild injury and do not require either investigation or treatment. As clinicians we rely on decision rules to guide our thinking around neuroimaging. Could parents apply the same decision rules to see if attending PED was needed? Whether parents interpret questions within these algorithms in the same way as clinicians was unknown.
Charlotte and her colleagues looked at the similarity or inter-observer reliability between clinicians and parents of head injured children using the Pediatric Emergency Care Applied Research Network (PECARN) head injury algorithm. In this single centre observational feasibility study, children over 2 years old presenting within 24 hours of a head injury were prospectively recruited. Parents were given a questionnaire, with the PECARN criteria in lay-man’s language, to complete whilst awaiting assessment. Following assessment, the treating clinician completed a similar questionnaire, blinded to the parent’s answers.
57 children were included with a mean age of 5.8 years (SD 4.07). The study found that:
- The most common mechanism of injury was a fall from standing (46%)
- Arrival GCS was 15/15 in nearly all (98%) children
- The inter-rater reliability between parents and clinicians for individual PECARN criteria was highly variable.
Kappa (K) values statistically present inter-observer reliability: 1.00 shows perfect agreement, 0 represents no agreement / equal to chance and any minus value indicates less agreement than chance.
- K values ranged for the PECARN criteria from -0.04 to 0.85
- There was poor agreement on whether the child displayed signs of altered mental status or bruising consistent with a base of skull fracture
- There was almost perfect agreement on whether there had been any loss of consciousness or vomiting
Charlotte’s take home message:
There is high variability in the agreement between clinicians and parents using PECARN criteria to assess the same child with a head injury. Whether differences are due to interpretation of words or the child requires further work but these findings have significant implications for public facing algorithms, such as those used by NHS 111.
Contact Charlotte about this work:
Contact Charlotte on twitter @charkennedyEM if you are interested in this research and would like to know more.
The work that was shortlisted for the Elizabeth Molyneuz prize and summarised here shows that the future of research in PEM is bright. I particularly want to congratulate Charlotte Kennedy who was awarded the Elizabeth Molyneuz prize by the judging panel at the conference in October. I hope that this work (along with the research presented in our Rod Little prize blog) helps to inspire both those currently conducting EM research and those thinking about getting into research. It really is an exciting time to be involved in driving our specialty forward.
References
- Kawasaki t. Update on pediatric sepsis: a review. Journal of Intensive Care (2017) 5:47
- Maitland K, Kiguli S, Opoka R, Engoru C, Olupot-Olupot P, Akech S, et al. Mortality after Fluid Bolus in African Children with Severe Infection. N Engl J Med 2011; 364:2483-2495
- Inwald DP, Canter R, Woolfall K on behalf of PERUKI (Paediatric Emergency Research in the UK and Ireland) and PICS SG (Paediatric Intensive Care Society Study Group), et al. Restricted fluid bolus volume in early septic shock: results of the Fluids in Shock pilot trial. Archives of Disease in Childhood 2019;104:426-431
- British Medical Association. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers. London: BMA, 2004.