Author: Jonathan M Jones / Editor: Steve Fordham / Reviewer: Mohamed Elwakil / Codes: / Published: 10/05/2021
Caveat
While the theory contained in this session provides useful knowledge about airway management, putting this knowledge into practice requires extensive supervised practical experience. Such experience can be reinforced and developed by courses such as the UK TEAM course upon which this session draws extensively.
Airway management in an elective situation is usually straightforward. Any difficulties in airway maintenance and ventilation prior to endotracheal intubation are usually dealt with by simple repositioning manoeuvres and the use of adjuncts[1]. Laryngoscopy usually provides a clear view of the cords and intubation itself is easy.
In the time critical environment of the emergency department, the scenario is complicated by:
- Limited scope for prior assessment
- The often poor physiological reserve of the patient
- The potential for a range of pathologies which may still be rapidly evolving
The failure rate for rapid sequence intubation in the emergency department is about 1%, with a cricothyroidotomy rate varying from 0.5% (medical patients) to 2.3% (trauma)[2]. Awareness of indicators of difficulty and techniques to deal with problems can reduce the complication rate[3].
For the purposes of this session the following definitions are used:
Difficult airway is being used to describe:
- Problems with bag-valve mask ventilation (BVM) despite repositioning and use of adjuncts, as covered in the session Basic Airway Management in the Adult
- Difficulties in intubation when attempted by a competent airway practitioner
Failed intubation is the inability to successfully place an endotracheal tube after three attempts by a competent airway practitioner[4].
Can’t intubate, can’t oxygenate (CICO) is when a failed intubation is compounded by an inability to maintain adequate oxygen saturation with BVM.
An individuals airway may be rendered difficult by:
Poor Preparation
Poor preparation may include:
- Inadequate positioning
- Poor availability of equipment
- Lack of suitable personnel
- Inadequate training
Normal anatomical and physiological variation may include:
- Facial hair
- Shape of jaw
- Abnormal teeth or lack of teeth
- Limited mouth opening
- Size of tongue
- Length and mobility of neck
- Position of larynx
- Pregnancy
Pathological anatomical variation may include:
- Soft tissue swelling as a result of burns, allergy/angio-oedema, infection and haematoma
- Maxillofacial trauma
- Cervical spine deformity or immobility, for example ankylosing spondylitis
- Obesity
- Abdominal distension
Clinical assessment
In the emergency situation there may be very little time for a considered clinical assessment but even the briefest of glances may be sufficient to alert the wary practitioner to potential hazards.
An obese, bearded, immobilised trauma patient with facial injuries may challenge an expert.
Six features have been identified as likely to cause difficulty with BVM ventilation in elective patients[6,7]:
- Presence of a beard
- Lack of teeth
- Age >55
- BMI >30
- History of snoring
- Inability to protrude the mandible so that the lower incisors are anterior to the upper incisors
Elective patients who prove both difficult to ventilate and difficult to intubate have been noted to have the last three from the above list plus a history of sleep apnoea and/or a particularly thick or obese neck[6].
The potential hazards identified, and others, have been incorporated into two mnemonics from the American Emergency Airway Management course.
MOANS acts as an aide-memoire for indicators of difficult BVM:
- M: Mask seal – for example a beard or blood
- O: Obesity and obstruction
- A: Age
- N: No teeth
- S: Stiff lungs
LEMON highlights patients who may be difficult to intubate:
- L: Look: a rapid gut-feeling assessment
- E: Evaluate the 3-3-2 rule
- M: Mallampati score see note below
- O: Obesity/obstruction (stridor in particular is worrying)
- N: Neck mobility

A normal patient should be able to accomodate:
 3 finger breadths between incisors
3 finger breadths between incisors
3 fingers from the tip of the chin to the neck
2 fingers from the chin/neck junction to the thyroid cartilage.

Note: Mallampati score is assessed, conventionally, by asking a seated patient to open their mouth as far as they can. This can be approximated in the supine patient using a tongue depressor or laryngoscope blade if necessary. If only the base of the uvula, or less, can be visualised, intubation may be more challenging. It is difficult to assess in the immobilised or obtunded patient [8].
Refresh your airway anatomy, watch this video:
The time critical nature of emergency airway scenarios mandates that the team be very familiar with their environment and roles.
A difficult airway trolley should be present with the equipment necessary to follow locally agreed guidelines. This will include alternative airway devices and equipment for establishing a surgical airway (Fig 1).
A variety of new devices for airway management have been developed in recent years including:
- Fibreoptic stylets
- Video laryngoscopes
- Optically enhanced laryngoscopes
Video laryngoscopes vs DIRECT?
The advent of video laryngoscopy has led to some experts stating that it should be considered standard of care (a loaded term) or at least best practice. this had led to vigorous and sometimes heated debate, especially in the emergency medicine community.[13]
All departments should have access to video laryngoscopy equipment Scott Weingart.[14]
Learning Bite
If a difficult airway is anticipated, the most experienced practitioner available must be present.
Learning Bite
Difficulty with an airway must be recognised early.
It is vital that the practitioner recognises when he or she is having problems and adopts an appropriate management strategy immediately. The temptation to struggle on without calling for assistance must be resisted.
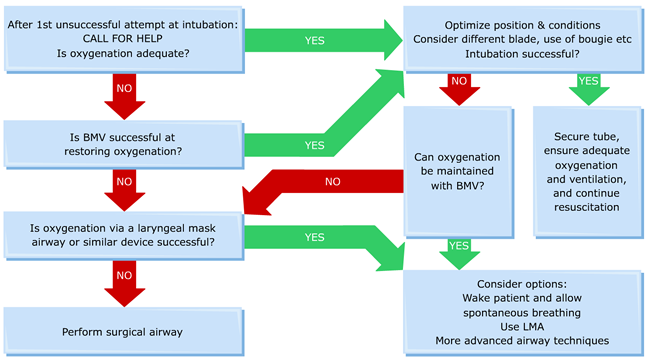
The management strategy presented here is an abbreviated adaptation of that which is taught on the UK TEAM course. Other similar algorithms have been published in the emergency medicine literature and merit consideration[11].
Learning Bite
All airway practitioners must have a simple algorithm for the management of the difficult airway and cant intubate/cant ventilate situations.
Airway management is fraught with difficulties. These include:
- Failing to be prepared well in advance of a potential difficult airway situation
- Not recognising that an airway may be difficult or may become difficult soon (e.g. upper airway burns)
- Being falsely reassured by a lack of indicators of difficulty
- Not calling for help early
- Pursuing attempts to place an endotracheal tube rather than maintaining oxygenation
- Capnography should be used wherever tracheal intubation is undertaken and remember No Trace=Wrong Place [13]
- Not recognising when a cant intubate/cant ventilate scenario has arisen and there is an immediate need for a surgical airway
- An airway may be rendered difficult by a host of factors both pathological and anatomical (Evidence grade D)
- While a number of features may indicate that a particular airway may be difficult, their absence does not mean that it wont be (Evidence grade D)
- If a difficult airway is anticipated the best airway practitioner available should be present (Evidence grade D).
- An airway that appears uncomplicated may deteriorate rapidly as pathology (e.g. thermal injury or haemorrhage) worsens (Evidence grade D)
- The resuscitation room is a time critical environment preplanning for management of the difficult airway is essential (Evidence grade D)
- Maintenance of oxygenation is more important than the presence of a tube in the trachea good bag mask valve technique is the most important airway skill (Evidence grade D)
- All airway practitioners must have a simple algorithm for the management of the difficult airway and cant intubate/cant ventilate situations (Evidence grade D)
- All airway practitioners must be capable of performing a cricothyroidotomy (Evidence grade D)
- If attempts to intubate have failed and ventilation is not possible by BVM or LMA a surgical airway must be obtained immediately (Evidence grade D)
- Walls RM, Murphy MF editors. Manual of emergency airway management. 3rd ed. Philadelphia: Wolters Kluwer, Lippincott Williams and Wilkins
- (Same as 1)
- Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: a justification for incorporating the ASA Guidelines in the remote location. J Clin Anesth 2004; 16:508516
- Nee PA, Benger J, Walls RM. Airway management. Emerg Med J 2008;25:98-102
- Ollerton JE, Parr MJA, Harrison K, Hanrahan B, Sugrue M. Potential cervical spine injury and difficult airway management for emergency intubation of trauma adults in the emergency department a systematic review. Emerg Med J 2006;23:3-11
- Khertepal S, Han R, Tremper K, Shanks A, Tait A, OReilly M, Ludwig T. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology 2006;105(5):885-891
- Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, Riou, B. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:12291236
- Levitan RM , Everett WW , Ochroch EA . Limitations of difficult airway prediction in the emergency department . Ann Emerg Med . 2004;44:307313
- Benger J, Nolan J, Clancy M eds. Emergency Airway Management. Cambridge University Press, 2008. ISBN: 9780511451591
- Yentis S, Predicting trouble in airway management (editorial view). Anesthesiology;2006:871-872
- Carley SD, Gwinnutt C, Butler J, Sammy I, Driscoll P. Rapid sequence induction in the emergency department: a strategy for failure. Emerg Med J 2002:19:109-113.
- Shehzad A and Cadogan M, Mallampati Score. Life in the FastLane, 2020.
- Nickson Ch, Direct versus Video Laryngoscopy. Life in the FastLane, 2020.
- Weingart S, Podcast 94 Has Video Laryngoscopy Killed the Direct Laryngoscope?. EMCrit. March 3, 2013. [Accessed on January 7th 2021].