Author: Richard J Parry / Editor: Jason M Kendall / Reviewer: Mohamed Elwakil Codes: A5 / Published: 19/06/2021
Definitions
Peripheral neuropathy is a pathological process affecting a peripheral nerve or nerves (includes cranial nerves). The term peripheral neuropathy encompasses any disorder of the peripheral nervous system and includes mononeuropathies, polyneuropathies, mononeuritis multiplex and radiculopathies.
Mononeuropathy describes the involvement of a single nerve and is usually due to a local cause such as trauma or entrapment.
Mononeuritis multiplex refers to multiple non-contiguous nerve trunks being affected simultaneously and is usually due to multiple infarcts of the vasa nervorum due to a systemic vasculitic process.
Polyneuropathy is diffuse symmetrical glove and stocking loss of peripheral nerve function, usually progressing proximally. (The terms peripheral neuropathy and polyneuropathy are sometimes incorrectly used interchangeably).
Radiculopathy is a pathological process affecting nerve roots.
Sensory, motor, sensorimotor (i.e. mixed) and autonomic systems may be affected.
The causes can be either inherited or acquired. Acquired peripheral neuropathies can be broadly sub-divided into those caused by disease and those caused by physical injury.
Presentation may be either acute/sub-acute (e.g. traumatic, GuillainBarr syndrome) or chronic (e.g. diabetic sensorimotor peripheral neuropathy).
Context
Why should we as Emergency Physicians be interested in peripheral neuropathy?
- Peripheral neuropathy is commonly encountered in our patient population
- Identifying peripheral neuropathy as a symptom or sign of disease may aid in the diagnosis of that underlying disease
- Diagnosing acute peripheral neuropathies are particularly important to the emergency physician GuillainBarr syndrome is the commonest cause of acute symmetrical peripheral polyneuropathy and can be fatal
- Acute mononeuritis multiplex is also a neurological emergency. The commonest cause is vasculitis and prompt treatment with steroids can prevent irreversible nerve damage
- It is a distressing symptom for which a number of treatments are available, some of which may be started in the emergency department. Important secondary prevention measures should also be considered
Prevalence
Evidence, albeit scarce, has shown a prevalence of peripheral neuropathy to be 2.4% amongst the general population increasing to 8% with advancing age.
Peripheral neuropathy affects approximately two thirds of diabetics irrespective of whether they are insulin or non-insulin dependent.
The most common type of generalised polyneuropathy is diabetic sensorimotor polyneuropathy. Leprosy is the commonest cause of polyneuropathy worldwide. Neuropathies associated with HIV infection account for an increasing number of cases.
Causes
The causes of peripheral neuropathies can be classified into broad categories (Fig 1):
There are seven aetiologies that account for almost all cases of peripheral neuropathy in the UK. These are shown below.
- Trauma
- Diabetes
- Malignancy
- Vitamin B12 deficiency
- Vitamin B deficiency (primarily alcoholics)
- Drugs
- Idiopathic (10-20%)
Pathophysiology
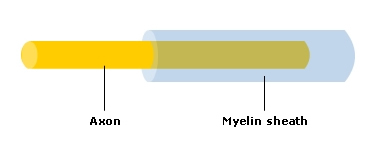
The peripheral nerve consists of 2 main cells the anterior horn cell with its axon and the Schwann cell that envelops the axon. Blood supply is via the vasa nervorum.
There are 6 principal mechanisms of peripheral nerve damage:
1. Demyelination

Damage to Schwann cell causes myelin disruption and slowing of nerve conduction. Examples include GuillainBarr syndrome, diphtheria, hereditary sensorimotor neuropathies and Chronic Inflammatory Demyelinating polyneuropathy (CIDP).
2. Axonal degeneration
The axon dies back from the periphery. Examples include Diabetes, metabolic conditions and toxic neuropathies such as drugs and alcohol.
3. Wallerian degeneration
Changes occurring after division of a nerve, for example after traumatic section of the nerve.
4. Compression
Changes occurring after nerve entrapment, for example Carpal tunnel syndrome.
5. Infarction
Microinfarction of vessels supplying the nerve, for example in diabetes and polyarteritis nodosa.
6. Infiltration
Nerves infiltrated by inflammatory cells.
History and examination
Attention should be paid to:
- The signs and symptoms of the peripheral neuropathy
- The consequences of these
- The underlying cause
Signs and symptoms / consequences of peripheral neuropathy
Different aetiologies may be associated with altered sensation, burning pain, weakness or autonomic features or a combination of these.
(i) Sensory failure leads to distal numbness, tingling, or burning of the extremities in the typical glove and stocking distribution, ascending proximally. Patients may struggle to perform tasks requiring sensory feedback such as doing up buttons.
Peripheral neuropathies most commonly produce sensory deficits. Examination should focus on identifying sensory loss in the various modalities: light touch, vibration, joint position sense and pain and temperature.
The consequences of sensory loss:
- Cuts and burns on the fingers/hands
- Charcots joints, where joints are damaged by trauma as a result of the loss of protective pain sensation. This especially affects the tarsal bones in diabetics leading to joint swelling and deformity, but without pain on movement
Conditions with predominantly sensory failures include:
- Diabetes mellitus
- Vitamin B12 deficiency
- Small cell carcinoma of the lung
- Renal failure
(ii) Motor examination will typically reveal peripheral nerve (ie. lower motor neuron) signs:
- Weakness
- Wasting
- Reduced tone
- Reduced or absent reflexes
- Fasciculations
Learning Bite
Attributing upper motor neuron (UMN) signs to peripheral neuropathy. UMN signs include weakness without atrophy, absence of fasciculations, increased tone and exaggerated reflexes.
Conditions with predominantly motor failure include:
- Guillain-Barr syndrome
- Porphyria
- Lead poisoning
- Diphtheria
Cranial nerve neuropathies might include a mixture of sensory and motor signs e.g.:
- Difficulty swallowing
- Difficulty speaking
- Double vision
(iii) Autonomic signs include:
- Postural hypotension
- Urinary incontinence
- Diarrhoea (occasionally constipation)
- Abnormal sweating
- Impotence
- Diminished pupillary responses
Conditions which can exhibit autonomic neuropathy include:
- Diabetes mellitus
- Amyloidosis
- Renal failure
- GuillainBarr syndrome
Symptoms and signs associated with the underlying causes of peripheral neuropathy:
- The underlying aetiology must be explored in the history enquiring about conditions such as diabetes, vitamin deficiency, alcoholism, offending medications, toxin exposure etc.
- Associated events should be sought such as Campylobacter infection which may precede GuillainBarr syndrome, unintentional weight loss suggesting carcinomatous neuropathy or arthralgia in connective tissue disease
- Family history may reveal genetic causes and a sexual history may suggest HIV
- Pain is typical of neuropathies due to diabetes or alcohol
- The time course of events is important
- General examination will identify other signs such as evidence of anaemia, alcoholic liver disease, rheumatoid hands, a vasculitic rash in polyarteritis nodosa, a cachexic appearance in malignancy (necessitating a more thorough exam including breasts and genitals)
- The nerves themselves may be thickened and palpable in leprosy, Charcot-Marie-Tooth, and amyloidosis
Clinical presentation dependant on type of neuropathy
Mononeuropathies are typically caused by trauma, compressive forces or have a vascular aetiology. The history taken should reflect these possible aetiologies. In someone with acute common peroneal nerve palsy for example it would be important to ask about trauma to the lateral aspect of the knee. In patients presenting with carpal tunnel syndrome it would be prudent to ask about associated conditions such as pregnancy, obesity, hypothyroidism, acromegaly and rheumatoid arthritis. Vascular risk factors should be elicited, including whether the patient is diabetic or has a vasculitic condition etc.
Polyneuropathies have a heterogeneous set of causes. Their presentation varies depending on the underlying pathophysiology. The speed of progression of the polyneuropathy coupled with its nature (axonal or demyelinating) can help identify its aetiology.
In acute demyelinating polyneuropathies such as GuillainBarr syndrome, motor nerve fibres are predominantly affected with weakness rather than sensory loss being the earliest signs of disease. In acute axonal polyneuropathies such as those caused by toxins, pain is the predominant component, which tends to worsen to a peak over 2-3 weeks, recovering over several months.
In chronic axonal polyneuropathies (eg. due to diabetes or renal failure) the symptoms usually begin in the toes before the fingers then spread proximally, as injury tends to be related to axonal length. Sensory symptoms tend to precede motor symptoms.
Sensory loss and weakness often present simultaneously in patients with chronic inflammatory demyelinating polyneuropathy (CIDP).
Mononeuritis multiplex can be distinguished from polyneuropathy as the multiple mononeuropathies in mononeuritis multiplex involve entirely non-contiguous nerves.
Features warranting a full evaluation[23]:
- Asymmetry
- Motor predominance
- Acute onset
- Prominent autonomic involvement
- Severe or rapidly progressive symptoms
- Sensory ataxia
Important clinical presentations
- Traumatic mononeuropathies
- Diabetes
- Vitamin deficiencies
- Drugs
- GuillainBarr syndrome
Traumatic mononeuropathies
Diabetic presentations
Diabetic patients commonly exhibit peripheral neuropathies. Sensory, motor and autonomic systems may be affected.
Sensory presentations can include unpleasant numbness, tingling and burning with aching in the lower limbs and feet, progressing over many months. There can be decreased sensation (especially vibration) in a glove and stocking distribution, absent ankle jerks or deformity (pes cavus, claw toes and rocker-bottom soles). Neuropathy is often patchy. The neuropathy often leads to painless punched-out plantar foot ulcers in an area of thick callous over pressure points, for example the metatarsal heads or the heel.
Diabetic amyotrophy (mainly motor, asymmetrical polyneuropathy) causes painful wasting of the quadriceps, and is potentially reversible with optimal glycaemic control.
Diabetic autonomic neuropathy leads to postural hypotension. Autonomic dysfunction amongst diabetics also causes diarrhoea (sometimes constipation). Bladder involvement causes loss of tone, incomplete emptying and stasis, predisposing to infection. Impotence may also occur.
Learning Bite
Do not make the assumption that if a diabetic patient can feel burning/aching pain in a limb, they do NOT have peripheral neuropathy in that limb.
Vitamin deficiency presentations
Vitamin B12 deficiency should always be excluded in a patient in whom any of the following are present:
- Peripheral sensory neuropathy
- Spinal cord disease
- Dementia
Initial symptoms are related to peripheral nerve damage numbness and tingling of extremities, signs of distal sensory loss with absent ankle jerks (owing to the neuropathy), combined with evidence of cord disease extensor plantars and exaggerated knee jerks (in which the posterior and lateral columns of the cord are damaged and the anterior columns remain unaffected), hence the term (sub-acute combined degeneration of the cord).
B12 deficiency occurs in any condition in which it is not ingested (vegan diet), Intrinsic factor is not produced (loss of functioning stomach), or its absorption is prevented (loss of/disease of the terminal ileum). In Pernicious Anaemia, the neurological changes are of particular importance because left untreated they can become irreversible.
Other vitamin deficiency syndromes
Vitamin B1 (thiamine) deficiency is seen in alcoholics and patients with a poor diet. Polyneuropathy is a feature because Vitamin B1 is involved in nerve conduction. Conditions associated with B1 deficiency include Beriberi and Wernicke-Korsakoff syndrome.
Vitamin B6 (pyridoxine) deficiency causes mainly a sensory neuropathy and is seen during isoniazid therapy for tuberculosis, in patients who are slow acetylators of the drug.
Vitamin B3 (nicotinic acid) deficiency is seen in carcinoid syndrome and alcoholism. Its deficiency is associated with dementia, dermatitis and diarrhoea the three Ds and this combination of features is seen in the clinical syndrome of pellagra.
Drug related peripheral neuropathy
GuillainBarr syndrome
GuillainBarr syndrome is an uncommon acute infective/inflammatory polyneuropathy. Campylobacter infection (diarrhoea +/- blood, fever, malaise, abdominal pain) is a recognised trigger for GBS. Other triggers include recent surgery, flu vaccination, or other non-specific viral illness (especially gastrointestinal or respiratory).
In GuillainBarr syndrome there follows a progressive acute symmetrical weakness starting in the legs and in some cases this ascends rapidly within days to involve the arms and trunk and then the intercostal muscles causing respiratory failure. Death can occur either as a result of rapidly progressing intercostal and phrenic nerve paralysis or autonomic dysfunction, leading to cardiac arrhythmias and haemodynamic instability.
Peripheral neuropathies must be distinguished from myopathies and neuromuscular junction disorders which also present with varying degrees of weakness and sensory loss. Myasthenia gravis, for example, (a neuromuscular junction disorder) is characterised by fatigability and tends to affect the proximal muscles and muscles innervated by the cranial nerves. Proximal weakness usually indicates a myopathy or neuromuscular junction disorder.
Focal sensory loss (in the absence of CNS pathology) suggests a peripheral neurological problem. A glove and stocking pattern of sensory loss suggests an axonal polyneuropathy. Nerve root lesions cause sensory loss in a dermatomal pattern. Numbness in a single nerve territory suggests trauma or entrapment neuropathy. Multiple areas of numbness in non-contiguous areas point to mononeuritis multiplex. Loss of reflexes occur with neuropathic lesions either affecting sensory or motor fibres.
Peripheral nervous system disease must be distinguished from central nervous system (CNS) disease (eg. stroke or spinal cord lesions). Signs and symptoms confined to a single limb usually suggest a peripheral aetiology. Associated pain in the extremity further increases the likelihood of peripheral pathology. Examination of deep tendon reflexes is the single most important test in determining whether a problem in central or peripheral. Brisk reflexes point to a central cause, whereas hyporeflexia or areflexia suggest a peripheral problem. CNS (upper motor neuron) lesions cause weakness which predominantly affects the extensor muscles of the arm and flexor muscles of the leg, and generalised increased tone. Atrophy of muscles and hypotonia isolated to a specific root or peripheral nerve, sites the pathology within the peripheral nervous system.
Investigations within the emergency department might include:
- Simple blood tests
- Full blood count
- Blood film
- ESR
- Urea and Electrolytes
- Liver function tests
- Thyroid function tests
- gamma-GT
- Glucose
- B12, folate
- Anti HIV antibodies
- CXR
- Urinalysis (for glucose, blood or protein)
- LP (raised protein level typical in GBS)
Further investigation may include tests for urinary Bence Jones protein, serum protein electrophoresis, autoimmune markers and lead levels.
Nerve conduction studies, electromyography (EMG), nerve biopsy, skin biopsy or genetic tests may be indicated.
Occasionally CT or MRI may be needed for example to detect vascular irregularities, herniated discs or spinal stenosis.
Treatment of peripheral neuropathy should involve:
- Treatment of the underlying cause
- Alleviation of symptoms
- Prevention of complications
Treatment of underlying cause
No curative treatments currently exist for inherited forms of peripheral neuropathy. Peripheral nerves have the ability to regenerate, as long as the nerve cell itself has not been killed. Treating the underlying cause of peripheral neuropathy can prevent new damage, for example, reducing exposure to toxins such as alcohol and avoidance of offending drugs. Rigorous glycaemic control in diabetics can help preserve nerve function. The emergency treatment of vitamin B12 deficiency involves 1 mg injections of vitamin B12 intramuscularly on alternate days until no further improvement (e.g. for 2 weeks), followed by maintenance treatment of 1 mg IM every 2 months for life. Complete neurological recovery is possible. If the neuropathy is due to a vasculitic process, prompt treatment with steroids can prevent irreversible nerve damage. Thyroid hormone replacement typically ameliorates the symptoms of hypothyroid polyneuropathy. Treatment of Guillain-Barr syndrome includes plasma exchange and intravenous immunoglobulin.
Treatment of symptoms
Neuropathic pain is often difficult to control. Simple analgesics (e.g. tramadol) may help to alleviate symptoms. Neuromodulators such as tricyclic antidepressants may have a beneficial effect.The best evidence of efficacy exists for gabapentin, carbamazepine, or topical capsaicin cream. Gabapentin for example may be started at a dose of 100 mg to 300 mg tds, then gradually increased to a total daily dose of 1800 mg. Local anaesthetics, injected or in patch form may help relieve more intractable pain. Occasionally nerves may be surgically destroyed. Surgery may help in other ways for example a mononeuropathy caused by a herniated disc may benefit from a microdiscectomy, or the symptoms of carpal tunnel syndrome should improve after surgical decompression.
Prevention of complications
Education, regular foot inspection, chiropody, soft shoes, and orthotics are important to avoid foot ulcers in patients with distal polyneuropathy.
The prognosis of a peripheral neuropathy clearly depends on its aetiology. Acute neuropathies such as Guillain-Barr syndrome appear suddenly, progress rapidly and resolve slowly as the damaged neurons heal. Chronic neuropathies begin subtly, progress slowly and may follow either a relapsing and remitting course, may reach a plateau phase or may slowly worsen over time.
As with any condition, it is important to ensure appropriate follow-up after the emergency department visit.
- Assuming peripheral neuropathy just affects the sensory system. It also affects motor, autonomic nerves and cranial nerves
- Failing to appreciate how common peripheral neuropathy is amongst diabetics. Two-thirds are affected
- Making the assumption that if a diabetic patient can feel burning/aching pain in a limb, they dont have peripheral neuropathy in that limb
- Attributing UMN signs to peripheral neuropathy. UMN signs include weakness without atrophy, absence of fasciculations, increased tone and exaggerated reflexes
- Failing to recognise vitamin B12 deficiency as a cause for peripheral neuropathy in a patient with concomitant signs of dementia and spinal cord disease
- Not taking into account a patients medication list as a cause for their peripheral neuropathy
- Assuming that peripheral neuropathy is not a problem that needs to be addressed in the emergency department
Key Learning Points
- Peripheral neuropathy is a pathological process affecting a peripheral nerve or nerves (includes cranial nerves). The term peripheral neuropathy encompasses any disorder of the peripheral nervous system and includes mononeuropathies, polyneuropathies, mononeuritis multiplex and radiculopathies
- Polyneuropathy describes the diffuse, symmetrical, glove and stocking loss of neurological function. This usually progresses proximally, and can be sensory, motor, sensorimotor (i.e. mixed) or autonomic
- Peripheral neuropathy is common with a prevalence of 2.4% amongst the general population, increasing to 8% with advancing age (Grade A)
- Almost all cases of peripheral neuropathy in the UK can be attributed to trauma, diabetes, malignancy, vitamin B12 deficiency, vitamin B deficiency (primarily in alcoholics), drugs and idiopathic causes (Grade A)
- Peripheral neuropathy affects approximately two-thirds of diabetics (Grade A)
- Attention should be paid to the signs and symptoms of the peripheral neuropathy, the consequences of these and the underlying cause
- Peripheral neuropathies most commonly produce sensory deficits. Examination should focus on identifying sensory loss in the various modalities: light touch, vibration, joint position sense and pain and temperature.
- Peripheral neuropathies must be distinguished from myopathies and neuromuscular junction disorders which also present with varying degrees of weakness and sensory loss. Proximal weakness usually indicates a myopathy or neuromuscular junction disorder
- Peripheral nervous system disease must also be distinguished from central nervous system (CNS) disease (e.g. stroke or spinal cord lesions). Examination of deep tendon reflexes is the single most important test in determining whether a problem in central or peripheral. Brisk reflexes point to a central cause, whereas hyporeflexia or areflexia suggest a peripheral problem
- Diagnosing acute peripheral neuropathies are particularly important to the emergency physician. Guillain-Barr syndrome is the commonest cause of acute symmetrical peripheral polyneuropathy and can be fatal. Acute mononeuritis multiplex is also a neurological emergency. The commonest cause is vasculitis and prompt treatment with steroids can prevent irreversible nerve damage
- Vitamin B12 deficiency should always be excluded in a patient who exhibits signs and symptoms of peripheral sensory neuropathy, spinal cord disease or dementia (Grade D)
- Investigations in the ED should include simple blood tests, chest x-ray and urinalysis (Grade D)
- Treatment of peripheral neuropathy should involve treatment of the underlying cause, alleviation of symptoms and prevention of complications
- Martyn CN, Hughes RAC. Epidemiology of peripheral neuropathy. J Neurology, Neurosurgery and Psychiatry 1997;62:310-318. Evidence 3b (as relates to UK practice)
- Dyck PJ et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy and nephropathy in a population-based cohort. The Rochester Diabetic Neuropathy Study. Neurology 1993;43:817. Evidence A 1a
- BMJ Publishing group. British National Formulary, March 2007. Evidence D
- Longmore M et al. Oxford Handbook of Clinical Medicine, 2001. 5th edn. Evidence D
- Simmons Z, Feldman MD. The pharmacological treatment of painful diabetic neuropathy. Clinical Diabetes volume 2000;18. Evidence D
- Cohen KL, Harris S. Efficacy and safety of nonsteroidal anti-inflammatory drugs in the therapy of diabetic neuropathy. Arch Intern Med 1987;147:1442-1444. (placebo controlled single blind crossover study) Evidence B 2a
- Max MB et al. Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology 1987;37:589-596 (double-blind placebo controlled trial). Evidence A 1a
- McQuay HJ et al. (1996) A systematic review of antidepressants in neuropathic pain. Pain 1996;68:217-227. meta-analysis of 21 different clinical trials. Evidence A 1a
- Backonja M et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA 1998;280:1831-1836. Evidence A 1b
- Capsaicin Study Group. Treatment of painful diabetic neuropathy with topical capsaicin: a multicenter, double-blind, vehicle-controlled study. Arch Intern Med 1991;151:2225-2229. Evidence A 1a
- Zhang WY, Po ALW. The effectiveness of topically applied capsaicin: a meta-analysis. Eur J Clin Pharmacol 1994;46:517-522 Meta-analysis of 4 randomised double-blind, placebo-controlled trials. Evidence A 1a
- Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: an update and effect related to mechanism of drug action. Pain 1999;83:389-400. Meta-analysis of placebo-controlled trials. Evidence A 1b
- Ryder REJ et al. An Aid to the MRCP PACES. 3rd edn. Blackwell Publishing, 2003. Evidence D
- Kunar P, Clark M. Clinical Medicine. 4th edn. WB Saunders, 1998. Evidence D
- Kelly P et al. MRCP 2 Success in PACES. 1st edn. Pastest, 2003. Evidence D
- Trend P et al. Neurology colour guide. 1st edn. Churchill Livingstone, 1992. Evidence D
- Moulton C, Yates D. Lecture notes: Emergency Medicine. 3rd edn. Blackwell Publishing, 2006. Evidence D
- Kalra PA. Essential revision notes for MRCP. 1st edn. Pastest, 1999. Evidence D
- Chan-Tack KM. eMedicine Botulism. September, 2008. Evidence D
- Newton E. eMedicine Myesthenia Gravis. March, 2007. Evidence D
- National institute of neurological disorders and stroke peripheral neuropathy fact sheet, Nov 2008. Evidence D
- Hughes RA. Clinical Review, Peripheral Neuropathy. BMJ 2002;324:466-469. Evidence D.
- Callaghan BC, Price RS, Feldman EL. Distal Symmetric Polyneuropathy: A Review. JAMA 2015; 314:2172.








