Author: Rebecca Mersh, James Vassallo / Editor: Rob James, Lauren Fraser / Codes: / Published: 06/01/2020
What is triage?
The word triage originates from the French word trier, meaning to sort. In the medical context, this sorting is of patients, by priority, for initial treatment and subsequent transport to a facility where more definitive care is available. (1) Triage is a common feature of Emergency Departments (EDs) in their provision of day-to-day emergency care, where RCEM guidelines suggest that patients have a brief assessment within 15 minutes of arrival in order to be prioritised appropriately (2).
What is a mass casualty incident (MCI)?
A medical MCI is any situation in which medical resources, such as personnel and equipment, are overwhelmed by the number and severity of casualties (3). This may be a relatively small incident in a resource-limited environment, but is more commonly considered in the context of larger-scale disasters such as the 2017 fire at Grenfell Tower or the Manchester Arena bombing.
Why is triage so important in MCIs?
Where demand for medical assistance and resources is greater than that available, the priority must be to identify those who are most in need of medical attention. Effective triage is therefore paramount in these situations aiming to allow ordered prioritisation in what is likely to be a chaotic situation.
Within the UK, triage at a major incident is performed in two stages. The initial primary triage assessment will take place at the scene of the incident and should take no more than 30 seconds per patient. The purpose of this primary process is to rapidly identify those patients who need a life-saving intervention. It is usually executed using an algorithm such as the Modified Triage Sieve MPTT-24. This is designed to be rapid, reliable and reproducible irrespective of the provider performing it. It is followed by a secondary triage process, which typically takes place in a more permissive environment (e.g. casualty clearing station) and is performed by a more experienced clinician. A number of different secondary triage processes exist, including the MIMMS Triage Sort, Anatomical Triage and Clinician Gestalt (1).
During triage in a mass casualty incident, patients are grouped into the following categories of decreasing treatment priority:
- Immediate: Casualties who are in need of life-saving interventions and require immediate treatment .
- Urgent: These casualties are unwell but with a degree of stability. They are unable to walk but have comparatively normal physiology. Typically, they will require treatment/interventions within 2-4 hrs.
- Delayed: Sometimes referred to as the walking wounded these casualties are, by definition, able to ambulate to a treatment area and are deemed safe to have a treatment delay of 4 hours or more.
- Expectant: These casualties have such severe injuries that they are unlikely to survive with the resources available and their treatment would divert effort away from patients with a greater chance of survival; they are therefore given the lowest priority for management. Invoking the P4 category requires Gold authority (usually ministerial level) in a UK incident.
In the UK military, the prefix T is usually added to these categories; in civilian emergency services the prefix P is used.
| Description | T/P | Colour |
| Immediate | 1 | Red |
| Urgent | 2 | Yellow |
| Delayed | 3 | Green |
| Expectant | 4 | Blue |
| Dead | Dead | Black or White |
Fig 1: Triage priority categories
The expectant category can be ethically and emotionally difficult. It is only used where resources are overwhelmed despite implementation of the normal mass casualty plan. If adequate resources become available these casualties will be treated as T1. It is important to remember the advice of the World Medical association that:
It is unethical for a physician to persist, at all costs, at maintaining the life of a patient beyond hope, thereby wasting to no avail scarce resources needed elsewhere (4).
Triage cards
As seen in Fig.1, categories also have an associated colour code. Following their assessment, casualties are given a triage card which displays this colour, allowing easy identification of those requiring the most urgent care. There are a variety of different cards available for this purpose; the SMART Tag folded cards of the style shown below are most commonly seen at UK mass casualty incidents. These have space for basic note keeping as well as providing the visual display of the patients triage category.

Fig 2: An example of commonly used SMART Tag triage cards. Available here.
Where triage cards are not available, patients may be labelled with the appropriate category number on their forehead.
It is key to note that triage is a dynamic process. As such regular re-assessment is required and if a patients clinical condition changes at any time, their priority category should be changed accordingly.
Primary Triage
The purpose of primary triage at a major incident is not to provide medical care but rather to identify patients in need of life-saving intervention by other healthcare providers. There are generally two exceptions to the triage not treatment rule (5):
- Provision of basic airway manoeuvres/adjuncts if a patient is not breathing
- Application of a Combat Application Tourniquet (CAT) for catastrophic haemorrhage
The MPTT-24
Primary triage, commonly referred to as the triage sieve, is generally performed using a validated algorithm such as the Modified Physiology Triage Tool (MPTT-24) (6). This has advantages in that it does not need to be performed by a person with a high level of medical training and could be effectively delegated to any competent person at the scene of the incident. It may in fact be advantageous for team members with less medical knowledge to undertake primary triage, as they are more likely to comply with the protocol and less likely to be distracted by other tasks or interventions. The triage sieve aims to be objective and readily reproducible. However, in common with all tools of its type, it does not take account of a patients likely course and may miss patients who are wholly salvageable for example a patient with airway burns may initially be walking and triaged a P3, but a short time later develop airway occlusion, and may die if they are not quickly identified and re-triaged for more urgent care.
The MPTT-24 triage tool can be seen below to be a simple flow chart. It considers the presence or absence of catastrophic haemorrhage, the patients ambulatory status, their responsiveness, and simple observations of their pulse and respiratory rate. Following the algorithm through, it is evident that with a maximum of six questions, the patient can be easily allocated to their triage category. They are immediately marked and (with the exceptions noted above), the person performing triage moves on to assess the next patient without executing any medical intervention.
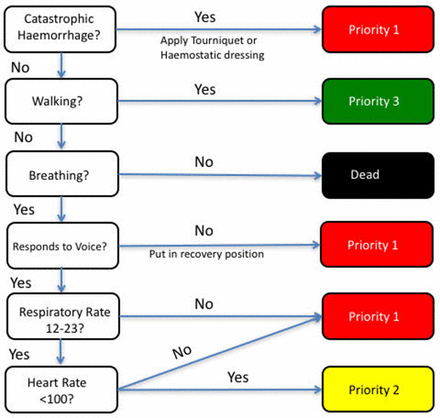
Fig 3: MPTT-24 Modified Physiological Triage Tool (6)
Secondary Triage
When time and resources allow, a secondary, more detailed triage assessment is made. It may be performed at the scene if evacuation times are prolonged, or more commonly occurs at the casualty clearing station or on a patients arrival to hospital (7). Perhaps a key difference in secondary triage is that, where appropriate personnel are available, clinician judgement is allowed. This would capture patients such as the airway burns case considered above.
The triage sort
A number of different methods exist to perform the secondary triage process. Most commonly known is the Triage Sort, as taught by MIMMS. This is derived from the Triage Revised Trauma Score (T-RTS) which was originally designed in the 1980s in the US to identify those patients who needed to be transferred to a major trauma centre. To use the Triage Sort, three physiological variables are assessed and given a score; the sum of these three scores is then used to derive the triage category.

Fig 4: Triage Sort Tool (8)
It is obvious that the triage sort aims to consider the casualty’s condition in more detail. It may therefore lead to their reassignment to a different triage category, either higher or lower than that initially allocated. This should be noted and triage card updated as required.
Controversies in secondary triage
Recent evidence demonstrates that within a UK civilian trauma population, the primary triage tools (MPTT-24 and NARU sieve) have a greater sensitivity than that of the Triage Sort and are quicker to perform. Alternative secondary triage tools are currently being researched and are likely to replace the triage sort tool above in the near future (9). However, the tool described here is currently still in common use and is taught on the UK Major Incident Medical Management and Support (MIMMS) course, so is included for completeness.
Paediatric Triage
Children and infants are commonly involved alongside adults in disasters or MCIs (10). Triaging of paediatric patients is challenging; due to the different normal physiological values for paediatric patients, the triage algorithms described previously are not appropriate, and different tools must be remembered. Paediatric triage is also emotionally challenging, and even when using the appropriate tools discussed below, there is a tendency for healthcare personnel to overtriage children at the expense of more unwell adults.
Paediatric Triage Tape
A simple way to combat some of the challenges of triaging paediatric casualties is with the use of paediatric triage tape. This can be used to measure the casualty’s length from heel to top of head, and the estimated weight as well as a triage sieve algorithm with suitably adjusted values, can be read off the tape at the appropriate point.

Fig 5: Use of paediatric triage tape
JumpSTART algorithm
If a paediatric triage tape is not available, clinicians can substitute age-adjusted physiological variables in the adult triage sieve tool themselves. This does, however, depend on the clinician being able to accurately estimate the patients weight, and also remember the normal values for heart and respiratory rate for a number of different age brackets. A perhaps simpler alternative is the JumpSTART Pediatric MCI Triage Tool (11) and this is advocated within the 2018 NHS England Clinical Guidelines for Major Incidents. This avoids the need for weight calculations or estimations and may be used for any patient who appears to be a child. The JumpSTART algorithm is as follows:
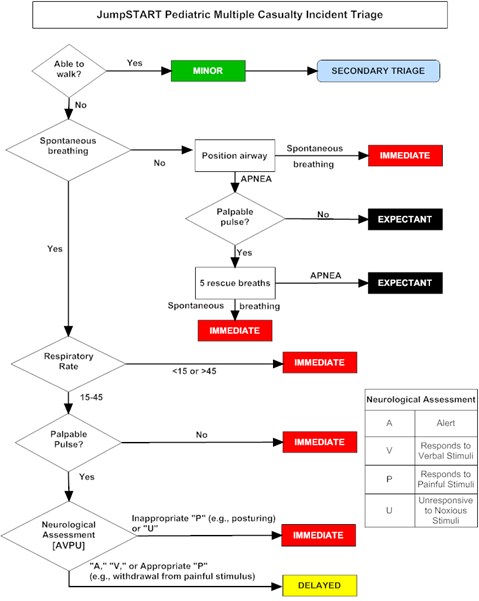
JumpSTART paediatric triage algorithm (11)
It is clear from this flowchart that the JumpSTART algorithm considers similar physiological parameters to the MPTT24 adult triage tool discussed above, however to account for the variability of normal physiological values in paediatric patients, a broader normal range for respiratory rate is used, and simply the presence or absence of a pulse as the cardiovascular measure. Studies have shown this tool to be easily remembered by clinicians and to improve accuracy of triaging paediatric patients (12).
However, the evidence to support any of the existing paediatric major incident triage tools is limited, with both the Paediatric Triage Tape and the JumpSTART method having poor sensitivity at identifying children in need of life-saving interventions (42% and 1% respectively) (13). Work is currently ongoing within the UK to try and identify a bespoke paediatric primary major incident tool that demonstrates improved performance at identifying those children who need life-saving interventions.
There are a number of problems which can arise even when patients are triaged appropriately using the previously discussed tools.
Similar to a diagnostic test, each triage tool will have its own performance characteristics. With triage tools being comprised of simple physiological assessments (even the Triage Sort) it is impossible for them to achieve 100% sensitivity and specificity. This is unsurprising given that they are expected to perform across the age range, in complex patients, potentially with multiple comorbidities/polypharmacy, in situations arising from a variety of mechanisms of injury. As such, in any incident there will be a number of patients who are ‘under-triaged’ – meaning that they are allocated to a lower priority than they should – or ‘over-triaged’ to a more urgent category than is appropriate.
In most situations in medicine, it would be deemed better to have patients ‘over-triaged’ thereby receiving care more urgently than they are strictly requiring – than ‘under-triaged’ and receiving delayed attention. However, in the case of a mass casualty incident this brings its own problems. Where resources are limited, having a greater number of patients allocated to receive urgent care may result in overwhelming of resources and a situation that is very difficult to manage, especially as there is no way of identifying the most critical patients within the T1/P1 pool. (8)
It is also important to be mindful that the triage system is in its nature a ‘snapshot’ assessment, considering a patient’s condition at just one point in time. As such, a casualty may be effectively compensating at the point of triage but subsequently deteriorate, and their stable physiology at the moment of assessment may put them at risk of not receiving the care that they require. Conversely a casualty may become much more stable following simple interventions or the passage of time after a stressful event, and if not reassessed appropriately they would continue to be prioritised for care despite it no longer being urgent for them. The value of revisiting the triage assessments for casualties such as these is clear however the practicalities of performing repeated triage assessments in what is by definition a resource-limited environment, are challenging. (14)
- Greaves, I. and Porter, K. (2010). Oxford handbook of pre-hospital care. 3rd ed. Oxford: Oxford University Press, p.602. (Greaves and Porter, 2010)
- RCEM guidelines. (2017). Initial Assessment of Emergency Department Patients. [online] Available here. [Accessed 30 Jul 2019].
- Marx, John A. Marx. (2014). Rosens Emergency Medicine: Concepts and clinical practice. 8th ed. Philadelphia, PA: Elsevier/Saunders.
- World Medical Association. (2010). Statement on medical ethics in the event of disasters. [online] Available here. [Accessed 7 Jul 2019].
- Sanders, M. and McKenna, K. (2011). Mosbys Paramedic Textbook. Burlington, MA: Jones & Bartlett Publishers.
- Vassallo, J., Smith, JE., and Wallis LA. (2018). Major incident triage and the implementation of a new triage tool, the MPTT-24. Journal of the Royal Army Medical Corps, 164(1), pp.103-106.
- NHS England. (2019). Clinical Guidelines for Major Incidents and Mass Casualty Events. [online] Available here. [Accessed 30 Jul 2019].
- Lowes A. and Cosgrave J. (2016). Prehospital organization and management of a mass casualty incident. BJA Education. [online] Available here. [Accessed 30 Jul 2019].
- Vassallo J. and Smith J. (2019). Major incident triage and the evaluation of the Triage Sort as a secondary triage method. Emergency Medicine Journal, 36(1), pp.281-286.
- Lyle, K., Thompson, T. and Graham, J. (2009). Pediatric Mass Casualty: Triage and Planning for the Prehospital Provider. Clinical Pediatric Emergency Medicine, 10(3), pp.173-185.
- CHEMM. (2011). JumpSTART Pediatric Triage Algorithm. [online] Available here. [Accessed 27 Jul 2019].
- Sanddal, T., Loyacono, T. and Sanddal, N. (2004). Effect of JumpSTART Training on Immediate and Short-term Pediatric Triage Performance. Pediatric Emergency Care, 2(11), pp.749-753.
- Wallis, L. (2006). Comparison of paediatric major incident primary triage tools. Emergency Medicine Journal, 23(6), pp.475-478. 14. Assistant secretary for preparedness and response. (2019). Mass Casualty Trauma Triage: Paradigms and Pitfalls. [online] Available here. [Accessed 2 Aug 2019]
